Healthcare plans can be so difficult to understand. During this 12 part series, Understanding your Insurance, we are breaking down each segment to enable you to make more informed healthcare decisions. Last month we examined Premiums, Deductibles and Co-Pays. There are 2 more elements that are crucial to understanding the basics of your healthcare plan, Coinsurance and Out-of-Pocket Maximums.
However, your out-of-pocket maximum is $7150. Therefore, you will only owe $2150 in coinsurance because that will get you to your out-of-pocket maximum amount of $7150. At this point, any additional covered medical costs you incur throughout the rest of the year will be covered by your insurance 100%. A copay is a set amount you pay for a service. A coinsurance is a percentage of the full cost of a service. Those payments and your deductible payments count toward your out-of-pocket maximum.1 Your out-of-pocket maximum helps protect you financially if you get sick or injured. The out-of-pocket maximum, also called OOPM, is the most you will have to pay out of your own pocket for expenses under your health insurance plan during the year. If you are a current BCBSTX member, you can see what your plan’s OOPM is within Blue Access for Members.
Coinsurance
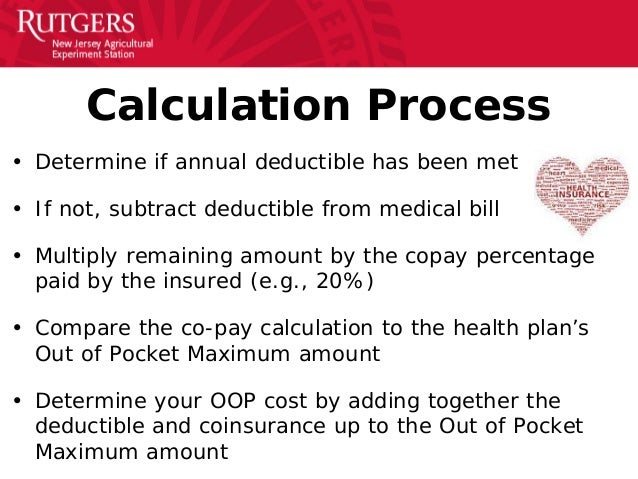
Coinsurance is your share of costs for healthcare services. Coinsurance usually kicks in once you’ve met your deductible.
Let’s say your plan has a $5000 deductible, which you’ve hit. (Hitting your deductible means that you’ve paid both your monthly premiums and $5000 towards your deductible for the year.) Now, you are going in for an office visit that costs $200.
For the sake of this example, let’s say your plan does not require a copay. And let’s also say that your coinsurance amount is 80/20, meaning once you’ve hit your deductible, your insurance covers 80% of the cost of the visit/procedure and you cover 20%.
Deductible = $5000—paid in full
Coinsurance = 80/20 (plan pays 80%, you pay 20%)
Flash plugin 8 downloadkeyclever. Office Visit Cost = $200
Amount due = $40
Maximum Out Of Pocket Limits
In this example, you should receive a bill for $40 and your insurance will pick up the rest. So this means that even though you have reached your deductible, you will still incur medical costs. That is, until you reach your out-of-pocket maximum.
Out-of-pocket maximum
This number is pretty important; it is the most you have to pay for covered healthcare services in a year. This figure does not take into account services you receive that are not covered under your healthcare plan or your monthly premium. However, it does include your deductible, copays and coinsurance payments for the year. Out-of-pocket maximums usually differ between an individual and a family so make sure to familiarize yourself with your particular plan and options. People generally reach their out-of-pocket maximums during a year with high medical costs. Below is an example of how this all plays out:
Let’s say you need to have a surgery that will cost $20,000.
Your plan specifications are as follows: Opposite gameelementary p.e. games.
- Deductible: $5000
- Coinsurance: 20%
- Out-of-pocket maximum: $7150
You pay the first $5000 of covered medical expenses towards your deductible.
Now, you owe your coinsurance amount on the rest of the medical costs of $15,000 for a total of $3000.
This brings you to a total of $8000. However, your out-of-pocket maximum is $7150. Therefore, you will only owe $2150 in coinsurance because that will get you to your out-of-pocket maximum amount of $7150. At this point, any additional covered medical costs you incur throughout the rest of the year will be covered by your insurance 100%. However, you are still required to pay your monthly healthcare premium as that is not included in your out-of-pocket maximum.
Do You Pay Copay After Out Of Pocket Maximum Is Met Bcbs
There we have the basics of healthcare costs incurred with healthcare coverage and medical visits. Next month we will explore what it means to be covered under more than one plan, or Coordination of Benefits.
Category: Uncategorized
Understanding the basic terminology of your health insurance is vitally important for patients with Pulmonary Hypertension. As a consumer of health care you need to understand how the system works and the language the insurance company uses to describe their coverage.
Deductible
A deductible is the amount of money that the patient must pay before their insurance begins to cover anything. However, there are certain exceptions to this (at least as of November 20, 2016). Under the Affordable Care Act, your insurance is required to pay for certain preventative care items prior to your deductible. This includes vaccinations and annual exams, mammograms and certain other items such as laboratory tests that are part of preventative care. Deductible amounts can vary widely from a few hundred dollars to thousands of dollars (these are referred to as high deductible plans).
Copay
A copay is the amount of money that the patient is required to pay when they check in for a visit. Over the years, the amount of copays has risen dramatically. Many plans have a lower amount for your primary care doctor and a higher amount for specialists. Copays do not count towards your deductible for most plans. However, as of 2014 copays do count towards your out of pocket maximum. As healthcare costs have risen, insurance companies have steadily increased the amount of copays. In the past, many plans had $10 co-pays. Now a copay of $75-100 is not uncommon.
Co-Insurance

Co-insurance is the percent of the bill that the patient must pay. For most insurance plans the co-insurance rate varies if the provider (or hospital/imaging center) is in network or not. For example, in-network co-insurance usually is 20% and out-of network co-insurance is 40%. This creates strong incentives for patients to use in-network facilities and doctors.
Out of Pocket Maximum
This simply means that after this amount is reached you have no further bills to pay.
Putting it Together with an Example
Let’s imagine that it is the beginning of the year (January 2nd) and I have to see my specialist for a problem. I check in with the receptionist and she asks for my copay of $50. Lesson plans totalitarianism on the rise. Next I see the doctor and check-out. A week later I receive a statement for $150 for the total visit charge. My insurance pays nothing because I have not yet met my $500 deductible. Because I have already paid $50 dollars in the co-pay I have $100 remaining to pay. It is worth noting that even though my insurance is not paying anything yet, the rates that the doctor charges are those agreed to by the insurance company. Now let’s fast forward to November the same year. It has been a difficult health year and I have had many doctor visits. I have met my deductible many months ago. Now I return to see my specialist again and I check in with the receptionist. I pay the $50 deductible. I see the doctor and a few weeks later I receive a bill for $150. I already paid $50 in the copay. Now I have 20% coinsurance on the remaining $100. My insurance will pay $80 and I will have to pay the remaining $20.

Now a week later I have an emergency surgery. My hospital bill comes to $20,000. Fortunately, I just met my out of pocket maximum. This means that for the remainder of the calendar year I will not have to pay anything for my health care. Due to a provision in the Affordable Care Act, since 2015 even prescription drug costs count towards the out of pocket maximum.
Deductible: amount you pay before your insurance starts paying (with certain exceptions)
Copay: amount you pay for each visit or test
Co-insurance: the percentage of the bill that the patient pays after the copay until the out of pocket maximum is reached
Out of pocket maximum: the most amount of money you will pay in a year
